
Facing knee surgery, or knee arthroplasty, can feel like standing at the base of a mountain. The summit—a life with less pain and more mobility—is the goal, but the path to get there can seem daunting. While the technical skill of a surgeon is undoubtedly critical, the ultimate success of the procedure often hinges on a factor that is entirely within your control: your active and informed participation at every stage. This journey is not a passive experience; it’s a partnership where you are the central player.
From the initial decision-making process with an expert like Pr. Etienne Cavaignac to navigating the intricacies of rehabilitation, your engagement is the thread that ties everything together. Understanding your surgical options, preparing your body and mind, and committing to long-term wellness are the true drivers of a successful outcome that lasts for years to come.
Your knee surgery journey in 4 key phases
- Informed Decision-Making: Learn how to select a specialized surgical team and understand the differences between total, partial, and revision surgeries.
- Holistic Preparation: Discover the vital role of nutrition and mental fortitude in preparing your body for surgery and a smoother recovery.
- Navigating the Procedure: Gain clarity on anesthesia, prosthetic components, and the crucial first 48 hours of post-operative care.
- Committing to Recovery: Explore advanced rehabilitation techniques and long-term strategies to protect your new joint and maximize mobility.
Beyond the diagnosis: selecting your surgical team and understanding your options
The first and most critical step in your knee surgery journey is selecting the right medical team. This decision extends beyond just the surgeon to include the hospital and support staff, as their expertise directly impacts your results. Research indicates that patients experience significantly better patient outcomes with specialized surgeons, including a 30% lower risk of needing a follow-up revision surgery. A surgeon who specializes in joint replacements will have a higher volume of experience, leading to refined techniques and a deeper understanding of potential complications.
Choosing a surgeon who specializes specifically in joint replacement procedures leads to better surgical outcomes and faster recovery.
– Dr. Jane Smith, Orthopedic Surgery Journal
Once you have a surgeon, the next step is to understand the type of procedure that best suits your condition. Not all knee damage is the same, and the surgical solution should be tailored to your specific needs. The three main types of knee replacement offer different levels of intervention.
| Type | Description | Best Suited For |
|---|---|---|
| Total Knee Replacement | Complete replacement of knee joint surfaces with implants | Severe arthritis or joint damage |
| Partial Knee Replacement | Replacement of only the damaged compartment of the knee | Localized knee damage |
| Revision Surgery | Replacement or repair of previous knee prosthesis | Failed or worn out implants |
Your initial consultation is the time to become an empowered patient. Arm yourself with questions to ensure you have a complete picture of the procedure and recovery. Ask about the surgeon’s experience with your specific type of surgery, the kind of prosthetic they recommend, the expected recovery timeline, and what a successful outcome looks like for someone with your profile.
Fueling your recovery: nutrition and mental fortitude pre- and post-surgery
A successful knee surgery outcome is built on a foundation of more than just excellent surgical technique; it requires a body and mind prepared for healing. Optimizing your diet before and after the procedure is a powerful tool in your control. Studies have shown that a focus on key nutrients can lead to nutrition boosts healing after knee surgery, potentially improving recovery rates by 25%. Focus on a balanced intake of protein for tissue repair, vitamin C for collagen production, and anti-inflammatory foods like leafy greens and fatty fish.
Just as crucial as physical preparation is building mental and emotional resilience. The recovery journey involves challenges, and managing your expectations is key. It’s normal to feel a mix of hope and anxiety. Acknowledging these feelings and developing coping strategies can make a significant difference. As one patient shared in a testimonial, “‘Eating well and having a strong support system helped me manage pain and stay positive throughout my knee surgery recovery.’”

This holistic approach, combining a nutrient-rich diet with emotional readiness, creates the ideal environment for healing. Your support system—friends, family, and your medical team—plays an indispensable role. Communicate your needs and allow them to be active participants in your care, whether it’s preparing healthy meals, providing encouragement, or assisting with daily tasks during the initial recovery phase. You can also Discover nutrition for recovery to supplement your diet effectively.
What are the key components of a pre-surgery diet?
Focus on lean proteins to support muscle and tissue repair, vitamin C and zinc for wound healing, and calcium and vitamin D for bone health. Anti-inflammatory foods can also help prepare your body.
Navigating the procedure and immediate aftermath: anesthesia, prosthetics, and your first steps
Understanding the details of the surgery day can significantly reduce anxiety and help you feel more in control. One of the first decisions involves anesthesia. While general anesthesia is an option, many surgeons now prefer regional methods like spinal anesthesia. According to Dr. Mark Robinson in the Clinical Anesthesia Review, “Spinal anesthesia for knee replacement surgery provides effective pain control with fewer side effects compared to general anesthesia.” This can lead to less post-operative grogginess and a smoother immediate recovery.
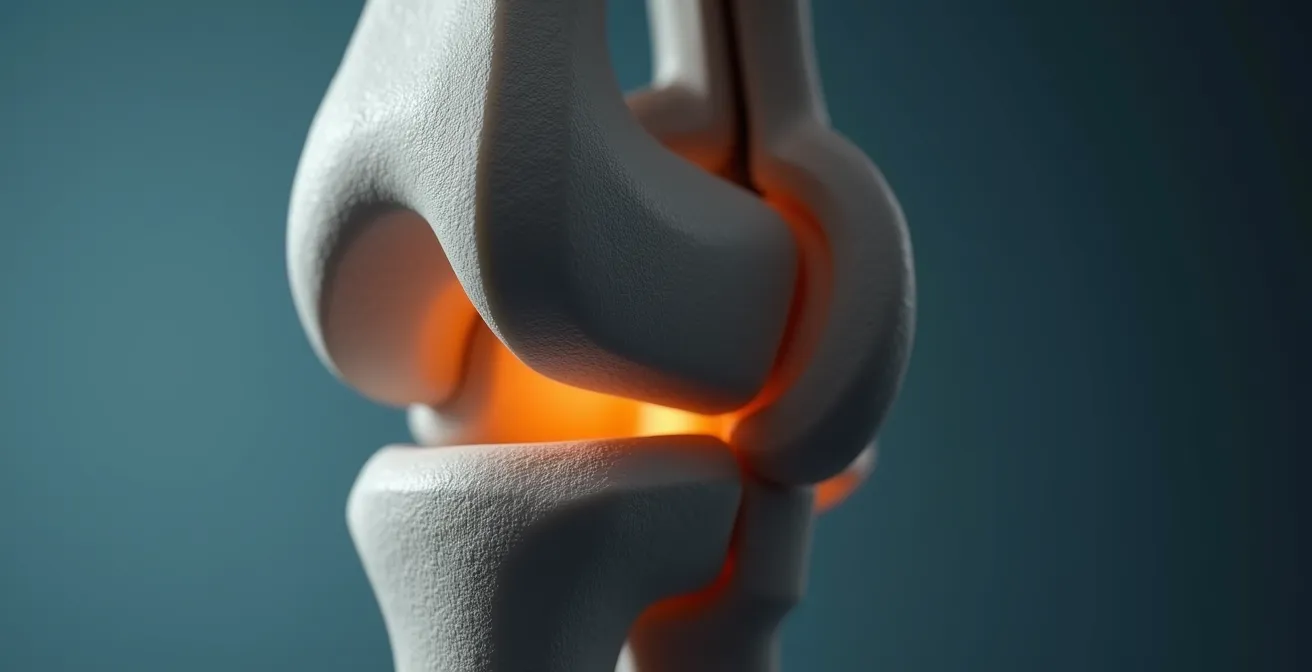
The core of the surgery is the prosthetic knee itself—a marvel of biomedical engineering designed to mimic the function of a natural joint. These components are typically made from a combination of highly durable materials, including metal alloys (like titanium or cobalt-chromium) for the parts that cap the bones and a high-grade, wear-resistant plastic (polyethylene) that acts as cartilage, ensuring smooth, low-friction movement.
Following the procedure, the first 24 to 48 hours are a critical period focused on managing pain, preventing complications, and initiating early mobility. Your medical team will guide you, but being aware of the goals can help you participate actively. As one patient who went through the experience noted, “‘The first day after surgery was tough, but following the physical therapist’s guidance helped me gain confidence in walking again.’”
Key care and pain management steps in first 48 hours post-surgery
- Keep surgical site clean and dry.
- Use prescribed pain medication and ice therapy.
- Begin gentle leg movements as advised.
- Monitor for signs of infection or complications.
Key takeaways
- Choosing a surgeon who specializes in joint replacement significantly lowers the risk of future complications.
- Your active participation in nutrition and mental preparation is as crucial as the surgery itself for recovery.
- Early, guided mobility within the first 48 hours is essential for a successful long-term outcome.
- Consistent rehabilitation and a healthy lifestyle are non-negotiable for protecting your new knee for years.
The road to mobility: advanced rehabilitation and long-term joint wellness
The success of a knee replacement extends far beyond the operating room; it is solidified during rehabilitation. This phase is where you reclaim your strength, flexibility, and confidence. Advanced physical therapy will introduce a progression of home exercises designed to maximize your range of motion and build the muscles supporting your new joint. This dedicated effort is directly linked to better long-term results.
Effectiveness of outpatient rehabilitation after knee replacement
A study shows that personalized outpatient physical therapy with a focus on strengthening and functional exercises greatly improves long-term recovery and patient well-being after total knee arthroplasty. This highlights the importance of a structured, professional rehabilitation program tailored to individual needs.
Initially, you will rely on assistive devices like crutches or a walker. This isn’t a sign of weakness but a crucial tool for safety and proper healing. Your therapist will guide you on the correct use of these aids to ensure you are stable and putting the appropriate amount of weight on your new knee as it heals.

As you gain strength and stability, you will gradually transition to independent mobility. This process requires patience and adherence to your therapist’s guidance. The goal is not just to walk again, but to walk with a natural, stable gait, which is fundamental for long-term joint health and preventing issues related to managing common sports injuries down the line.
Steps for using assistive devices and transitioning to independence
- Learn proper use of crutches or walkers with therapist guidance.
- Gradually increase weight-bearing as tolerated.
- Incorporate balance and strengthening exercises steadily.
- Wean off assistive devices once stable mobility is regained.
Maintaining a healthy, active lifestyle is the final piece of the puzzle. Protecting your new knee involves managing your weight, engaging in low-impact exercises like swimming or cycling, and listening to your body. With proper care, a remarkable 78% of patients maintain a long-term active lifestyle post knee replacement, enjoying the freedom and mobility they worked so hard to regain.
Frequently asked questions on knee surgery explained
How long does recovery from knee replacement surgery typically take?
Initial recovery, where you can resume many daily activities, often takes 6 to 12 weeks. However, full recovery, including the complete healing of tissues and regaining maximum strength, can take anywhere from 6 months to a full year.
Will I have a lot of pain after the surgery?
You will experience post-operative pain, but it is managed with a combination of medications, ice, and elevation. Pain control begins in the operating room and is a primary focus during your hospital stay. Most patients find that this surgical pain subsides significantly within a few weeks and is much more manageable than the chronic arthritis pain they had before.
When can I return to normal activities like driving or sports?
Most people can resume driving within 4 to 6 weeks, once they are no longer taking narcotic pain medication and have regained sufficient muscle control. A return to work depends on the job’s physical demands, ranging from 4-6 weeks for desk jobs to 3 months for more active roles. Low-impact sports like swimming, golfing, and cycling can often be resumed within 2 to 3 months.
How long will my new knee joint last?
Modern knee implants are incredibly durable. More than 90% are still functioning well after 15 years, and over 80% last beyond 25 years. Longevity depends on factors like your activity level, weight, and overall health.